 It’s amazing that something as small as a poppy seed can make you so sick. But ticks are doing just that. If you search “Lyme disease” on the Internet, you’ll find almost 13 million results. It’s staggering! And so are the climbing rates of new cases each year. Lyme disease is found all 50 states, and on every continent except Antarctica. Everyone is at risk, but young children ages 5-15 and adults age 40-65 have the most confirmed cases.
It’s amazing that something as small as a poppy seed can make you so sick. But ticks are doing just that. If you search “Lyme disease” on the Internet, you’ll find almost 13 million results. It’s staggering! And so are the climbing rates of new cases each year. Lyme disease is found all 50 states, and on every continent except Antarctica. Everyone is at risk, but young children ages 5-15 and adults age 40-65 have the most confirmed cases.
According to the CDC, Lyme disease is the fastest growing vector-borne, infectious disease in the United States (vector-borne diseases are transmitted among their human, animal, or plant hosts by arthropods, usually insects). In the U.S. alone, the CDC estimates that Lyme disease infects around 476,000 people a year, and recognizes that it is a tremendous public health problem in the country. This number is higher than the number of women diagnosed with breast cancer as well as the number of people diagnosed with HIV/AIDS each year in the U.S. Other groups have cited that they believe the number of new tick-borne cases per year could equal 1 million due to poor diagnostics.
Easy to Get, Hard to Diagnose & Treat
Lyme disease is easy to get, but can be difficult to diagnose and treat. Lyme disease is a multi-systemic illness transmitted through the bite of a tick. The disease itself is caused by the spirochete (SPY-ROH-KEET) Borrelia Burgdorferi. The Lyme spirochete can cause infection of multiple organs and produce a wide range of symptoms.
Lyme disease is prevalent across the U.S., and around the world. With Borrelia Burgdorferi alone, there are 5 subspecies with more than 100 strains in the US and 300 strains worldwide. Unfortunately it doesn’t stop there. Ticks are known to carry as many as 13 other bacteria, viruses and parasites, all with their own set of complex symptoms.
 You Will Not Feel A Tick Bite!
You Will Not Feel A Tick Bite!
Unlike mosquito or spider bites, you will not feel a tick bite. Ticks secrete a pain killer in their saliva which helps them go unnoticed. And because ticks are so small, you may never see a feeding tick on you. When ticks are done having their blood meal on you, they’ll drop off. What may be left is a small red bite mark, which might be itchy or hot. Symptoms can take anywhere from days, weeks, even months and years to manifest, depending on the infections the tick transmitted as well as the strength of your immune system.
50% or Less Recall Tick Bite/Get Bulls-Eye Rash
The International Lyme and Associated Diseases Society cites that fewer than 50% of patients recall a tick bite, and fewer than 50% of patient recall any rash, particularly the classic bulls-eye rash or erythema migrans (EM). Atypical rashes are seen far more commonly than the red expanding-ring rash.
It is important to note that a bulls-eye rash is considered a diagnostic positive for Lyme disease in Pennsylvania and requires no further verification prior to starting an appropriate course of antibiotic therapy.
Tick Risk
Ticks are active year-round. They do not die from frost or snow, but stay in leaf litter and wait for warmer weather to crawl out and up to look for a meal. Ticks do not know state borders, and your state of residence does not accurately reflect your Lyme disease risk. Ticks are found in many surprising settings—from forests to urban parks with lots of concrete and even desert areas in the west, on the way to your mailbox, at the edge of the highway and in your own yard. In fact, there is a statistic from the Tick Management Handbook published by the Connecticut Agricultural Experiment Station and authored by Kirby Stafford, III, Ph.D. that states 75% of all Lyme disease cases are picked up from ticks during activities around the home. Because ticks travel, you travel and pets travel, this creates a dynamic situation with many opportunities for exposure to Lyme disease.
Ticks Carry More than Just Lyme Disease!
Tick-borne diseases (bacteria, viruses, or parasites carried by ticks) are rapidly emerging. Anytime testing is done for Lyme disease, testing should be done for the presence of co-infections. If these co-infections are left untreated, their continued presence prevents successful treatment of Lyme disease. The chart below highlights diseases associated with several common ticks:
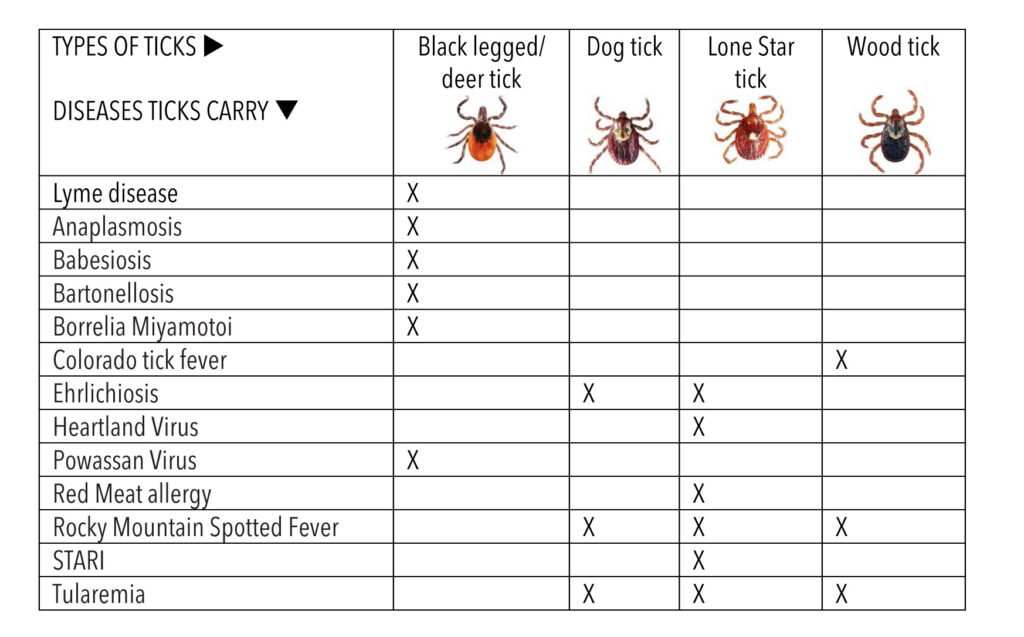
For more on tick-borne diseases in the U.S., visit https://www.cdc.gov/ticks/diseases/index.html
Symptoms of Tick-Borne Disease
Like Syphilis in the 19th century, Lyme disease has been called the great imitator because its symptoms mimic many other diseases. It can affect any organ of the body, including the brain, nervous system, muscles, joints and heart, according to LymeDisease.org. Symptoms include, but are not limited to:
- A rash
- Flu-like symptoms (fever, chills, sweats, nausea, muscle aches; be especially wary of any “summer” flu symptoms)
- Musculoskeletal: joint pain or swelling, muscle pain or weakness, burning in palms or soles of feet, bone sensitivity, tendonitis, fibromyalgia
- Neurological: persistent headaches, Bell’s palsy/facial drooping , tremors, pressure in the head, fainting, muscle twitching, constant low body temperature, diminished reflexes, restless leg syndrome
- Mental: memory loss, brain fog, declining performance at work/school, stammering/stuttering, disorientation, trouble finding the right words
- Physiological: mood swings, depression, anxiety attacks, insomnia, depersonalization
- Head, Face, Neck: stiff neck, dental pain, difficulty swallowing, sore throat, scalp rash
- Eyes/Visions: floaters, blurry vision, sensitivity to light, pressure in eyes
- Ears/Hearing: tinnitus, sensitivity to sound
- Digestive: abdominal pain, irritable bladder, frequent heartburn, GERD
- Respiratory/Circulatory: shortness of breath, persistent head congestion, chest pains, night sweats, heart palpitations, heart block, heart murmurs, low blood pressure
There are several free resources for checking symptoms as well as your likelihood of Lyme exposure:
- lymedisease.org/lyme-disease-symptom-checklist/
- https://cangetbetter.com/symptoms/
- https://projectlyme.org/resource/what-are-the-symptoms/
- globallymealliance.org/about-lyme/diagnosis/symptoms/
Lyme disease should be considered in the diagnosis of rheumatologic and neurologic conditions, as well as chronic fatigue syndrome, fibromyalgia, lupus, multiple sclerosis, Parkinson’s disease, Alzheimer’s disease, ALS, RA, Epstein bar virus infection, Crohn’s disease, carpal tunnel syndrome, TMJ and any difficult-to-diagnose multi-system illness. Because the diagnosis and treatment options for Lyme and other tick-borne infections are continually evolving, it is vital that patients and/or family and friends educate themselves and become an advocate for their health rights.
Lyme Disease Prevention Steps
Just like you apply sunscreen to protect against the sun’s harmful rays, protecting yourself from ticks can be just as easy. There is significant evidence that spraying your skin with tick repellent and clothing is the most effective way to reduce tick bites. Keep a bottle of repellent in your garage to make applying repellent part of your daily routine. Skin repellent spray can include natural or commercial products, always read the product safety labels. Socks and shoes, as well as pants, shirts, hats and other clothing, can be pre-sprayed outdoors and allowed to dry with Permethrin before moving it back indoors. Permethrin is an insecticide in the pyrethroid family that are synthetic chemicals that act like natural extracts from the chrysanthemum flower, that has been used. Permethrin kills ticks after they cross over the treated fabric. (NOTE: permethrin when wet can be toxic to cats and aquatic invertebrates and should not be used near bodies of water; always read product safety labels).
After being outdoors, leave your shoes in the garage if you can and run your clothing first in the dryer on HIGH HEAT for 10 minutes. This will kill any ticks, and then you can put the clothes in the washer. Be sure to do thorough tick checks on your body and run fingers through hair. Try to shower within two hours of exposure as showering can help wash off any loose ticks, especially in your hair. Once attached, ticks do not wash off in the shower.
 If a tick is already attached, the sooner you remove it the less risk of disease transmission. Proper tick removal includes using pointed tweezers to grab the tick as close to the skin as possible. Slowly and steadily pull straight up (do not twist, do not covers tick with anything attempting to smother it). Disinfect the bite. Save it in a sealed bag and send out to a lab for testing to know your disease risk (Ticklab.org offers free testing for PA residents).
If a tick is already attached, the sooner you remove it the less risk of disease transmission. Proper tick removal includes using pointed tweezers to grab the tick as close to the skin as possible. Slowly and steadily pull straight up (do not twist, do not covers tick with anything attempting to smother it). Disinfect the bite. Save it in a sealed bag and send out to a lab for testing to know your disease risk (Ticklab.org offers free testing for PA residents).
Learn more about prevention and take the simple steps that can protect yourself, your family and any pets from tick bites and tick-borne disease. A free Dare 2B Tick Aware prevention brochure series is available from PA Lyme Resource Network, funded by the Pennsylvania Department of Health. Additional resources for reliable information include:
- ILADS.org
- Lymedisease.org
- PALyme.org
- Ticklab.org (tick testing)
- Preventing Lyme Disease and Other Tick-Borne Infections, by Bob Oley
Disclaimer: The blog is for informational and educational purposes only. It is not intended to replace or supersede patient care by a healthcare provider. If an individual suspects the presence of a tick-borne illness, that individual should consult a healthcare provider who is familiar with the diagnosis and treatment of tick-borne diseases.






